Child Health
4 Things Parents and Youth Athletes Should Know About Concussions
Last Updated on November 12, 2024 by Daily News Staff
(Family Features) Despite the attention drawn to the topic of concussions over the past decade, it can be difficult to find readily available answers about what parents and young athletes should do after sustaining a concussion.
The Katsuyama family started 2023 without a single concussion, even with quite a few hockey and lacrosse seasons under its belt. That changed when Rylan, 11, received two concussions within five months from sports. One week after Rylan’s second concussion, his brother, Brandon, 13, was illegally checked from behind in a hockey game and sustained his first concussion. After clearing protocol in four weeks, he suffered a second concussion six weeks later.
Both boys endured months of headaches, missed school, dizziness, nausea and the added difficulty of navigating a significant injury peers and adults couldn’t see.
Their father, Brad Katsuyama, co-founder of IEX – a disruptive stock exchange featured in the best-selling book by Michael Lewis, “Flash Boys: A Wall Street Revolt” – sought out expert opinions to guide his family’s decisions and shares some acquired knowledge to help parents and athletes.
1. Brain injuries should be diagnosed by a concussion specialist.
There is no X-ray, MRI or CT scan that can show the extent of most concussion-related injuries, which makes diagnosing them subjective. Symptoms can also appear days after a hit. For example, Brandon was cleared by the emergency room after his first concussion, but two days later failed every test administered by a doctor specializing in concussions.
2. Rushing back to play is one of the worst mistakes you can make.
Experts consistently reinforced that coming back from a concussion too soon can significantly increase long-term brain injury risks. There is likely no tournament, playoff game or tryout worth this risk. An example of how to return smartly is Patrice Bergeron of the National Hockey League’s Boston Bruins, who sat out an entire year to properly heal from a concussion.
“Patrice had four more concussions over his career, and each one was less severe than the last,” renowned concussion specialist Dr. Robert Cantu said. “That wouldn’t have happened without recovery from the first one.”
3. Parents and kids need to be honest about symptoms.
The culture in youth sports praises toughness. Getting your “bell rung” and continuing to play can be viewed as a badge of honor. However, this same mentality can cause athletes to lie to parents, trainers and coaches to get back in the game, which can greatly increase long-term risks. Conversely, the same adults can unduly influence a potentially vulnerable player back on to the field of play. Proper diagnosis requires both adults and athletes to be level-headed and honest in their assessment of concussions.
4. Every person and every concussion is different.
One person’s history and experience with concussions seldom carries any relevance to the concussions experienced by another. For example, Katsuyama played varsity football, hockey and rugby for four years in high school and football in college.
“For the longest time, my definition of a ‘real’ concussion was blacking out, vomiting or pupils dilating,” Katsuyama said. “My sons had none of those symptoms after their hits, but it turns out the severity of their injuries were far greater than anything I had experienced.”
The Katsuyamas turned to the Concussion Legacy Foundation and the Cantu Concussion Center, in addition to their local concussion specialist, to advise their path forward, which has led them to racquet sports and golf in the near-term and long-term playing no more than one contact sport in a school year. Learn more at concussionfoundation.org.
Photo courtesy of Shutterstock
SOURCE:
Brad Katsuyama
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
News
Children can be systematic problem-solvers at younger ages than psychologists had thought – new research
Child psychologists: Celeste Kidd’s research challenges long-standing ideas from Jean Piaget about children’s problem-solving abilities. Her findings show that children as young as four can independently utilize algorithmic strategies to solve complex tasks, contradicting the belief that systematic logical thinking develops only after age seven. This insight highlights the importance of nurturing algorithmic thinking in early education.
Celeste Kidd, University of California, Berkeley
I’m in a coffee shop when a young child dumps out his mother’s bag in search of fruit snacks. The contents spill onto the table, bench and floor. It’s a chaotic – but functional – solution to the problem.
Children have a penchant for unconventional thinking that, at first glance, can look disordered. This kind of apparently chaotic behavior served as the inspiration for developmental psychologist Jean Piaget’s best-known theory: that children construct their knowledge through experience and must pass through four sequential stages, the first two of which lack the ability to use structured logic.
Piaget remains the GOAT of developmental psychology. He fundamentally and forever changed the world’s view of children by showing that kids do not enter the world with the same conceptual building blocks as adults, but must construct them through experience. No one before or since has amassed such a catalog of quirky child behaviors that researchers even today can replicate within individual children.
While Piaget was certainly correct in observing that children engage in a host of unusual behaviors, my lab recently uncovered evidence that upends some long-standing assumptions about the limits of children’s logical capabilities that originated with his work. Our new paper in the journal Nature Human Behaviour describes how young children are capable of finding systematic solutions to complex problems without any instruction. https://www.youtube.com/embed/Qb4TPj1pxzQ?wmode=transparent&start=0 Jean Piaget describes how children of different ages tackle a sorting task, with varying success.
Putting things in order
Throughout the 1960s, Piaget observed that young children rely on clunky trial-and-error methods rather than systematic strategies when attempting to order objects according to some continuous quantitative dimension, like length. For instance, a 4-year-old child asked to organize sticks from shortest to longest will move them around randomly and usually not achieve the desired final order.
Psychologists have interpreted young children’s inefficient behavior in this kind of ordering task – what we call a seriation task – as an indicator that kids can’t use systematic strategies in problem-solving until at least age 7.
Somewhat counterintuitively, my colleagues and I found that increasing the difficulty and cognitive demands of the seriation task actually prompted young children to discover and use algorithmic solutions to solve it.
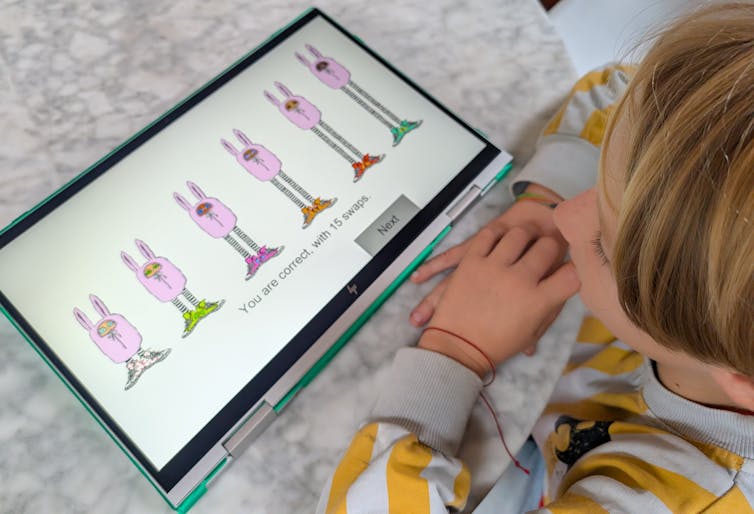
Piaget’s classic study asked children to put some visible items like wooden sticks in order by height. Huiwen Alex Yang, a psychology Ph.D. candidate who works on computational models of learning in my lab, cranked up the difficulty for our version of the task. With advice from our collaborator Bill Thompson, Yang designed a computer game that required children to use feedback clues to infer the height order of items hidden behind a wall, .
The game asked children to order bunnylike creatures from shortest to tallest by clicking on their sneakers to swap their places. The creatures only changed places if they were in the wrong order; otherwise they stayed put. Because they could only see the bunnies’ shoes and not their heights, children had to rely on logical inference rather than direct observation to solve the task. Yang tested 123 children between the ages of 4 and 10. https://www.youtube.com/embed/GlsbcE6nOxk?wmode=transparent&start=0 Researcher Huiwen Alex Yang tests 8-year-old Miro on the bunny sorting task. The bunnies are hidden behind a wall with only their sneakers visible. Miro’s selections exemplify use of selection sort, a classic efficient sorting algorithm from computer science. Kidd Lab at UC Berkeley.
Figuring out a strategy
We found that children independently discovered and applied at least two well-known sorting algorithms. These strategies – called selection sort and shaker sort – are typically studied in computer science.
More than half the children we tested demonstrated evidence of structured algorithmic thinking, and at ages as young as 4 years old. While older kids were more likely to use algorithmic strategies, our finding contrasts with Piaget’s belief that children were incapable of this kind of systematic strategizing before 7 years of age. He thought kids needed to reach what he called the concrete operational stage of development first.
Our results suggest that children are actually capable of spontaneous logical strategy discovery much earlier when circumstances require it. In our task, a trial-and-error strategy could not work because the objects to be ordered were not directly observable; children could not rely on perceptual feedback.
Explaining our results requires a more nuanced interpretation of Piaget’s original data. While children may still favor apparently less logical solutions to problems during the first two Piagetian stages, it’s not because they are incapable of doing otherwise if the situation requires it.
A systematic approach to life
Algorithmic thinking is crucial not only in high-level math classes, but also in everyday life. Imagine that you need to bake two dozen cookies, but your go-to recipe yields only one. You could go through all the steps of making the recipe twice, washing the bowl in between, but you’d never do that because you know that would be inefficient. Instead, you’d double the ingredients and perform each step only once. Algorithmic thinking allows you to identify a systematic way of approaching the need for twice as many cookies that improves the efficiency of your baking.
Algorithmic thinking is an important capacity that’s useful to children as they learn to move and operate in the world – and we now know they have access to these abilities far earlier than psychologists had believed.
That children can engage with algorithmic thinking before formal instruction has important implications for STEM – science, technology, engineering and math –education. Caregivers and educators now need to reconsider when and how they give children the opportunity to tackle more abstract problems and concepts. Knowing that children’s minds are ready for structured problems as early as preschool means we can nurture these abilities earlier in support of stronger math and computational skills.
And have some patience next time you encounter children interacting with the world in ways that are perhaps not super convenient. As you pick up your belongings from a café floor, remember that it’s all part of how children construct their knowledge. Those seemingly chaotic kids are on their way to more obviously logical behavior soon.
Celeste Kidd, Professor of Psychology, University of California, Berkeley
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Dive into “The Knowledge,” where curiosity meets clarity. This playlist, in collaboration with STMDailyNews.com, is designed for viewers who value historical accuracy and insightful learning. Our short videos, ranging from 30 seconds to a minute and a half, make complex subjects easy to grasp in no time. Covering everything from historical events to contemporary processes and entertainment, “The Knowledge” bridges the past with the present. In a world where information is abundant yet often misused, our series aims to guide you through the noise, preserving vital knowledge and truths that shape our lives today. Perfect for curious minds eager to discover the ‘why’ and ‘how’ of everything around us. Subscribe and join in as we explore the facts that matter. https://stmdailynews.com/the-knowledge/
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
Child Health
Your Child’s Oral Health: A Foundation for Better Overall Health
Good oral health is essential for children, and Medicaid and CHIP provide accessible dental coverage to eligible families, covering services like cleanings and fillings. Regular dental visits starting at age one can prevent cavities and build healthy habits. Families can check eligibility and find dentists through InsureKidsNow.gov.

(Feature Impact) Good oral health sets the stage for a lifetime of healthy smiles and better overall health. Medicaid and the Children’s Health Insurance Program (CHIP) help eligible families access affordable and comprehensive care for their children and teens, including regular cleanings, fillings, X-rays, and more to help ensure that eligible kids have access to essential dental services. By practicing good dental habits and seeing a dentist regularly, children can avoid dental problems and maintain healthy smiles as they grow.
Dental Coverage Available Through Medicaid and CHIP
If you’re looking for affordable dental coverage, your child may qualify for free or low-cost health insurance through Medicaid and CHIP. Together these programs cover more than 36 million children nationwide.
Enrollment is open year-round, and many families qualify even if they don’t realize it. Beyond dental care, Medicaid and CHIP also cover preventive health services, emergency care, vision care, prescriptions, and mental and behavioral health services for eligible children.
To see if your family is eligible and to find dentists in your area who accept Medicaid and CHIP, visit InsureKidsNow.gov and explore the “Find a Dentist” tool.
Start Good Dental Habits Early

Regular dental visits are an important part of your child’s oral health routine. Children should see a dentist by the age of 1 and continue with visits twice a year (every six months) as they get older. Going to checkups on a regular schedule can help catch problems early or before they even start. Cavities (also known as tooth decay) are the most common preventable chronic disease among children in the United States, and more than half of all children have cavities by the time they’re 6 to 8 years old. When left untreated, cavities can cause pain and infections that may affect eating, speaking, playing, learning – and even mental health.
The dental visit will vary depending on your child’s age and milestones, but it can include cleanings, full teeth and gum exams, treatments, and guidance on caring for your child’s teeth. Dental visits also help children become comfortable with the dentist, reducing anxiety, and building a positive relationship with oral health care that will benefit them throughout their lives.
Enrolling in CHIP and Medicaid
Medicaid and CHIP provide free or low-cost health coverage to eligible families and children. You can apply online, by phone, by mail, or in person directly at your state’s Medicaid agency. Learn more at InsureKidsNow.gov.
Provided by the U.S. Department of Health and Human Services at U.S. taxpayer expense.
Photos courtesy of Shutterstock
![]()
SOURCE:
Centers for Medicare and Medicaid Services
Our Lifestyle section on STM Daily News is a hub of inspiration and practical information, offering a range of articles that touch on various aspects of daily life. From tips on family finances to guides for maintaining health and wellness, we strive to empower our readers with knowledge and resources to enhance their lifestyles. Whether you’re seeking outdoor activity ideas, fashion trends, or travel recommendations, our lifestyle section has got you covered. Visit us today at https://stmdailynews.com/category/lifestyle/ and embark on a journey of discovery and self-improvement.
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
Child Health
Recognizing the Signs of Pediatric Growth Hormone Deficiency: How Early Recognition and Advocacy Helped One Family Find Answers
Diane Benke noticed her son Alex’s height concerns starting at age 7, despite his pediatrician’s reassurances. After persistent worries, they consulted an endocrinologist, leading to a diagnosis of Pediatric Growth Hormone Deficiency (PGHD). Following treatment changes, including a switch to weekly hormone injections, Alex’s growth improved, allowing the family to focus on their well-being.
Last Updated on February 5, 2026 by Daily News Staff
(Family Features) “Our concerns about Alex’s growth began around the age of 7,” said his mother, Diane Benke.
Though Alex measured around the 50th percentile for weight, his height consistently hovered around the 20th percentile. Benke’s instincts told her something wasn’t quite right.
“I kept asking our pediatrician if this could mean something more,” she said. “Each time, I was reassured that everything was fine. After all, I’m only 5 feet tall myself.”
At first, Benke tried setting her worries aside. Alex was one of the youngest in his class, and she wondered if he could simply be a “late bloomer.”
However, as Alex progressed through elementary school, particularly in the 4th and 6th grades, his height percentile dropped into the single digits. The height difference between Alex and his peers became impossible to ignore.
Despite Benke’s growing concerns, their pediatrician continued to assure them Alex was fine.
“We were told as long as he was making some progress on the growth chart, there was no need to worry,” she said, “but we were never actually shown the charts.”
It wasn’t until one of Benke’s friends confided that her own daughter had recently been diagnosed with Pediatric Growth Hormone Deficiency (PGHD) that she decided to seek an endocrinologist.
“Although it took several months to get an appointment,” Benke said, “we were determined to get more answers.”
Navigating the Diagnosis Process
Getting a diagnosis for many medical conditions can be a long journey. However, early detection and diagnosis of PGHD is important. It can help minimize the impact on overall health and support optimal growth.
Once Alex was seen by a pediatric endocrinologist, he underwent a series of evaluations, including bloodwork, a bone age X-ray to compare his chronological age with his skeletal age and a growth hormone stimulation test, which measures the body’s ability to produce growth hormone. He also had a brain MRI to rule out the potential of any pituitary abnormalities.
The results of these tests confirmed the diagnosis of PGHD, a rare condition that occurs when the pituitary gland does not produce enough growth hormone. PGHD affects an estimated 1 in 4,000-10,000 children.
Some common signs parents might notice include: their child being significantly shorter than other kids their age, slower growth rate over time, delayed puberty, reduced muscle strength or lower energy levels, slower bone development and delayed physical milestones.
“Receiving Alex’s diagnosis was a relief,” Benke said. “It provided clarity and a path forward.”
Moving Forward with Treatment
“While the diagnosis process was exhausting, starting treatment made the process worthwhile,” Benke said.
For decades, daily injections of a drug called somatropin, which is similar to the growth hormone your body produces, have been the standard of care for PGHD. It wasn’t until 2015 that the Growth Hormone Research Society recognized the need for a long-acting growth hormone (LAGH), offering once-weekly dosing as an alternative to daily injections.
Benke explained navigating the insurance approval process was another challenge.
“Our insurance required us to try a daily medication before approving a weekly option,” she said.
Alex spent three months on daily medication, often missing doses, before he was approved to switch to a weekly treatment option.
“The weekly option made such a positive impact,” Benke said. “We now have minimal disruptions to our daily routine and Alex hasn’t missed a single dose since.”
Beyond a more convenient dosing option, the change gave Benke peace of mind.
“We could focus more on being a family again, without the daily worries of his next dose,” she said.
If you’re concerned about your child’s growth, talk to their doctor as soon as possible. Early diagnosis is important, as treatment becomes less effective once a child’s bones stop growing.
Benke’s advice to other parents: “Trust your instincts. If something feels wrong, seek out a specialist and push for answers and don’t give up, even when faced with hurdles… Stay hopeful and persistent – it’s a journey worth fighting for.”
Visit GHDinKids.com to download a doctor discussion guide to help prepare for your next appointment.
SOURCE:
Skytrofa
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
