health and wellness
Hepatitis B shot for newborns has nearly eliminated childhood infections with this virus in the US
The hepatitis B vaccine for newborns, recommended since 1991, has significantly reduced U.S. childhood infections. Current CDC guidelines might change, potentially delaying vaccination, putting infants at risk. Vaccination at birth is crucial to prevent chronic infections and severe health outcomes.

Hepatitis B shot for newborns has nearly eliminated childhood infections with this virus in the US
David Higgins, University of Colorado Anschutz Medical Campus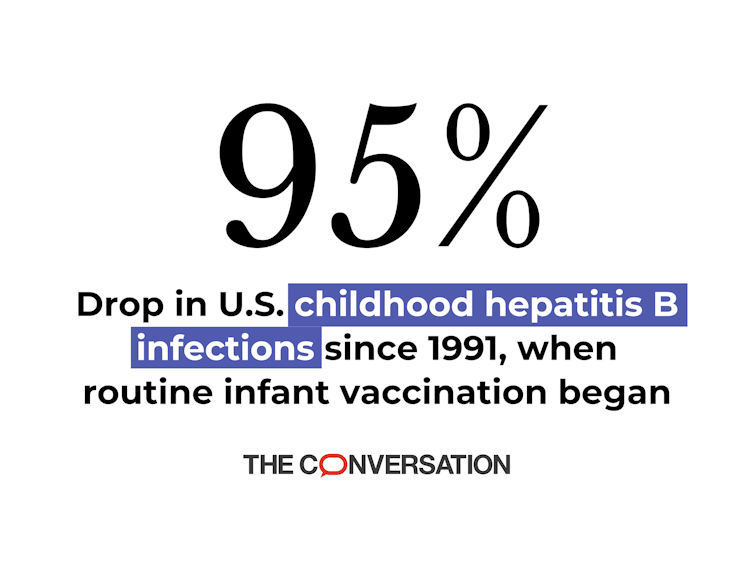
Before the United States began vaccinating all infants at birth with the hepatitis B vaccine in 1991, around 18,000 children every year contracted the virus before their 10th birthday – about half of them at birth. About 90% of that subset developed a chronic infection.
In the U.S., 1 in 4 children chronically infected with hepatitis B will die prematurely from cirrhosis or liver cancer.
Today, fewer than 1,000 U.S. children or adolescents contract the virus every year – a 95% drop. Fewer than 20 babies are reported infected at birth.
I am a pediatrician and preventive medicine specialist who studies vaccine delivery and policy. Vaccinating babies for hepatitis B at birth remains one of the clearest, most evidence-based ways to keep American children free of this lifelong, deadly infection.
On Sept. 18, 2025, the Advisory Committee on Immunization Practices, an independent panel of experts that advises the Centers for Disease Control and Prevention, debated changing the recommendation. According to the proposed language of the vote, infants whose mothers test positive for hepatitis B would still receive the vaccine at birth. Infants whose mothers do not test positive for hepatitis B would get the vaccine at 1 month of age, though parents would have the choice for them to receive it earlier. On Sept. 19, however, the committee tabled the vote, delaying it to the next committee meeting, scheduled for Oct. 22-23.
Although such a proposed change sounds small, it is not based on any new evidence. It would undo more than three decades of a prevention strategy that has nearly eliminated early childhood hepatitis B in the U.S.
While the committee regularly reviews vaccine guidance, nothing is business as usual about this meeting. In June 2025, Secretary of Health and Human Services Robert F. Kennedy Jr. disbanded the entire committee and handpicked new members. The committee has long-standing procedures to evaluate the evidence supporting the risks and benefits of a given vaccine, as well as other parameters of its use. But in this case, these procedures are not being followed.
Why the CDC adopted universal hepatitis B shots
Hepatitis B is a virus that infects liver cells, causing inflammation and damage. In adults, it is spread through blood and bodily fluids, which can happen through unprotected sex, contaminated needles or contact with open cuts or sores of someone who is carrying it.
The hepatitis B vaccine has been available since the early 1980s. Before 1991, public health guidance recommended giving newborns and young children the hepatitis B vaccine only if they were at high risk of being infected – for example, if they were born to a mother infected with hepatitis B or living in a household with someone known to have hepatitis B.
That targeted plan failed. Tens of thousands of children were still infected each year.
Some newborns were exposed when their mothers weren’t properly screened or if their mothers got infected late in pregnancy. Children also became infected through household contacts or in child care settings by exposures as ordinary as shared toothbrushes or a bite that breaks the skin. Because hepatitis B can survive for a week on household surfaces, and many carriers are unaware they are infected, even babies and toddlers of uninfected mothers remained at risk.
Recognizing these gaps, in 1991 the CDC recommended hepatitis B vaccination for every child starting at birth, regardless of maternal risk.
Vaccinating at birth
The greatest danger for infants contracting hepatitis B is at birth, when contact with a mother’s blood can transmit the virus. Without preventive treatment or vaccination, 70% to 90% of infants born to infected mothers will become infected themselves, and 90% of those infections will become chronic. The infection in these children silently damages their liver, potentially leading to liver cancer and death.
About 80% of parents choose to follow the CDC’s guidance and vaccinate their babies at birth. If the CDC’s recommendations change to delaying the first dose to 1 month old, it would leave babies unprotected during this most vulnerable window, when infection is most likely to lead to chronic infection and silently damage the liver.
The hepatitis B vaccines used in the U.S. have an outstanding safety record. The only confirmed risk is an allergic reaction called anaphylaxis that occurs in roughly 1 in 600,000 doses, and no child has died from such a reaction. Extensive studies show no link to other serious conditions.
The current recommendations are designed to protect every child, including those who slip through gaps in maternal screening or encounter the virus in everyday life. A reversion to the ineffective risk-based approach threatens to erode this critical safety net.
David Higgins, Assistant Professor of Pediatrics, University of Colorado Anschutz Medical Campus
This article is republished from The Conversation under a Creative Commons license. Read the original article.
STM Daily News is a vibrant news blog dedicated to sharing the brighter side of human experiences. Emphasizing positive, uplifting stories, the site focuses on delivering inspiring, informative, and well-researched content. With a commitment to accurate, fair, and responsible journalism, STM Daily News aims to foster a community of readers passionate about positive change and engaged in meaningful conversations. Join the movement and explore stories that celebrate the positive impacts shaping our world.
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
Lifestyle
How to Practice Thoughtful Grief Etiquette Online
Grief experts advise caution in sharing condolences and loss-related information on social media, emphasizing the importance of prioritizing the grieving family’s needs. Thoughtful posting practices include waiting for family approval, reaching out privately first, and avoiding speculation about the cause of death. Compassionate communication is essential in these sensitive situations.

(Feature Impact) News of a death can spread online in seconds – often before families have notified close family members privately. That’s why grief experts urge people to rethink how they share condolences, tributes and loss-related information on social media, particularly during the winter months when grief can feel especially isolating.
“Grief etiquette is about putting the needs of the grieving family first, not our urge to say something publicly,” said Dr. Camelia L. Clarke, National Funeral Directors Association (NFDA) spokesperson, funeral director and grief educator with nearly 30 years of experience. “Just because information can be shared instantly doesn’t mean it should be.”
Social media has become a common place for sharing condolences, tributes and memories. However, grief experts caution that, without thoughtful consideration, online posts can unintentionally cause harm. Knowing when to post, what to say and when to remain silent can make a meaningful difference for families experiencing loss.
Consider this advice from the experts at the NFDA.
Grief Etiquette in the Digital Age
Grief etiquette refers to the unspoken guidelines for how individuals acknowledge death, loss and mourning, particularly online.
According to Clarke, one of the most important principles is restraint.
“When a death is shared online too quickly, families can feel exposed and overwhelmed at a moment when they’re still processing the loss themselves,” she said. “Waiting is an act of compassion.”
Best Practices for Posting About Loss Online
As social media continues to play a role in modern mourning, grief professionals encourage users to pause before posting and consider a few key guidelines:
- Let the family lead. Don’t post about a death until the immediate family has made it public.
- Ask permission. Obtain consent before sharing photos, stories or tributes.
- Reach out privately first. A direct message, call or handwritten note can be more meaningful than a public comment.
- Avoid speculation. Don’t ask about or share details regarding the cause of death.
- Offer ongoing support. Grief extends far beyond the first days or weeks after a loss.
What to Say (and Avoid)
When expressing condolences online, experts recommend simplicity, sincerity and sensitivity. Messages that acknowledge loss without attempting to explain or minimize it are often the most supportive.
Helpful phrases include:
- “I’m sorry for your loss.”
- “Thinking of you and your family.”
- “I’m here if you want to talk or need anything.”
By contrast, well-meaning cliches can unintentionally cause harm. Phrases such as “They’re in a better place” or “Everything happens for a reason” may reflect the speaker’s beliefs, but they can feel dismissive to someone grieving.
“Grieving people don’t need answers – they need presence,” Clarke said. “Listening matters more than saying the perfect thing.”
Resources for Families and Friends
As digital spaces continue to shape how people communicate during life’s most difficult moments, experts agree empathy, patience and respect remain timeless.
“Grief is deeply personal,” Clarke said. “When we slow down and lead with compassion, we honor both the person who has died and those who are left to grieve.”
To learn more about how to support a grieving person and access free, expert-reviewed resources for navigating grief, expressing condolences and supporting loved ones before, during and after a loss, visit RememberingALife.com, an initiative of the NFDA.
Photo courtesy of Shutterstock
<img src="https://ssl.google-analytics.com/collect?v=1&tid=UA-482330-7&cid=1955551e-1975-5e52-0cdb-8516071094cd&sc=start&t=pageview&dl=http%3A%2F%2Ftrack.familyfeatures.com%2F17832%2F10240&dt=HOW-TO-PRACTICE-THOUGHTFUL-GRIEF-ETIQUETTE-ONLINE" />
<img src="https://erp.featureimpact.com/api/v1/tracking/17832/10240/track.gif" />SOURCE:
National Funeral Directors Association
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
Food and Beverage
Fresh Thinking About Frozen: Bring Quality Meals to the Table While Cutting Food Waste and Stretching Your Budget
For many families, the freezer is for last-minute meal options. However, new federal nutrition guidance and growing scientific consensus reveal a different reality: frozen foods can be the starting point for healthy eating, not a backup plan.
Last Updated on February 21, 2026 by Daily News Staff
(Feature Impact) The key to easy preparation of high-quality meals, wasting less food and saving money may already be sitting in your kitchen.
For many families, the freezer is for last-minute meal options. However, new federal nutrition guidance and growing scientific consensus reveal a different reality: frozen foods can be the starting point for healthy eating, not a backup plan. That’s why the American Frozen Food Institute (AFFI) is launching “Fresh Thinking About Frozen,” a campaign to help families discover these benefits of frozen foods.
Making Nutrition Achievable
The recently released 2025-2030 Dietary Guidelines for Americans, the nation’s top nutrition advice, emphasizes portion control and nutrient-dense foods. Frozen options deliver on both counts.
Families who keep frozen produce on hand tend to eat more fruits and vegetables overall. Pre-portioned frozen meals also help people eat what they need without overdoing it. Plus, the convenience factor matters: frozen berries are ready for a morning smoothie, pre-cut frozen vegetables can be added to tonight’s stir-fry and a balanced frozen meal can be quickly paired with a salad.
That isn’t cutting corners. It’s being smart on how best to feed a family well.
Freezing Hits the Pause Button on Fresh Foods
Freezing food only changes a food’s temperature, not its nutrition. Freezing keeps food close to its original state without requiring additives.
Produce begins to lose nutritional value right after it’s harvested. Freezing fruits and vegetables hours after harvest pauses nutrient degradation and locks in the vitamins and minerals, so the food remains farm fresh even as it travels across the country to your grocery store. Frozen meals are similarly made with real ingredients and turned into just-cooked recipes then frozen for families to eat when they’re ready.
The nutrition community understands this. A recent survey conducted by AFFI found 94% of registered dietitians agree frozen fruits and vegetables are just as nutritious as their fresh counterparts. Another 92% said frozen foods offer a variety of nutritious meal offerings. These findings are central to the “Fresh Thinking About Frozen” message: Frozen is not second-best. It’s simply smart.
Solving the Food Waste Problem
Nearly 40% of food in the United States gets thrown away, according to the nonprofit ReFED. That translates to roughly $1,500 per year per household, straight into the trash along with unused produce and forgotten leftovers.
Frozen helps fix that problem. Eight in 10 consumers agree buying frozen helps reduce food waste at home, AFFI research finds. The reason is simple: You use what you need, when you need it and the rest stays perfectly preserved. No more dreading the refrigerator cleanouts and feeling guilty over the uneaten food going into the trashcan.
Time for Fresh Thinking
Families already making this shift aren’t settling for less. They’re strategic about nutrition, budget and time. They integrate the freezer into regular meal planning. They feel confident about providing quality foods that are simply frozen.
The freezer isn’t a place of last resort. It’s a tool for eating well in real life. Visit frozenadvantage.org/FTAF for tips, recipes and resources to make the most of your freezer.
Photos courtesy of Shutterstock
SOURCE:
American Frozen Food Institute
At our core, we at STM Daily News, strive to keep you informed and inspired with the freshest content on all things food and beverage. From mouthwatering recipes to intriguing articles, we’re here to satisfy your appetite for culinary knowledge.
Visit our Food & Drink section to get the latest on Foodie News and recipes, offering a delightful blend of culinary inspiration and gastronomic trends to elevate your dining experience. https://stmdailynews.com/food-and-drink/
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
health and wellness
Stacking Healthy Habits for Progress, Not Perfection
Healthy Habits: Many struggle with building healthier habits due to unrealistic expectations rather than lack of motivation. The American Heart Association’s My Life Check tool offers personalized heart health insights, helping to set attainable goals. Simple lifestyle changes—focused on nutrition, movement, sleep, and stress management—can gradually lead to significant health improvements.

(Feature Impact) Despite the best of intentions, it’s common for plans to build healthier habits to fall flat. Often, the culprit isn’t a lack of motivation or discipline; rather, it’s unrealistic expectations.
Overhauling your lifestyle requires a level of commitment that isn’t always practical. Understanding your personal health needs and the challenges you need to overcome can help give you a more realistic roadmap toward better health.
Tools to Guide You
Every plan needs a starting point and there are many reputable sources that can help guide you toward a plan that addresses your personal health needs.
For example, the American Heart Association introduced My Life Check, a simple, free tool to help individuals understand their heart health and what’s driving it. Users answer simple questions about their daily habits and health factors to get a personalized Heart Health Score in minutes.
The results are private and downloadable, giving you full control of your information. The tool turns big goals into small, specific actions you can start right away. Knowing your numbers relative to your heart health (and where you are in comparison to target ranges for optimal health) can help you decide how to build a better map to get you where you want to be.
While the report is customized to each individual, no personal data is stored and answers are only used to calculate health scores and provide personalized recommendations and practical steps to improve your health, so you can use your results to focus on what matters most to you. Every small step you take, such as moving more, eating smarter, sleeping better or managing stress, can add up over time.
Finding Your Path
Once you’re armed with data and know where you stand on your heart health numbers, small steps become clearer and more manageable. That knowledge makes it easier to choose one area to focus on, such as getting more sleep, taking daily walks or adding more color to your meals.
Healthy changes don’t need to be expensive or complicated. The best habits are ones that fit real life when every action you take moves you closer to your goals.
Eat Smart
Choose foods that help you feel your best, one meal at a time. Add more color to your plate and focus on balance, not restriction. Simple, affordable swaps can make a real difference.
Move More
Find movement that fits your life, such as a walk, a stretch or dancing while you cook. Every bit of activity counts and it all supports your heart and mind. Move for joy, not just for results.
Sleep Well
Rest is a foundation of good health, not a reward. Protect your bedtime routine and give your body the recovery it deserves. Notice how good sleep makes everything else easier.
Manage Stress
Check in with yourself regularly, both mentally and emotionally. Create simple moments to pause, breathe, laugh or step outside. Connection, kindness and calm all support a healthy heart.
Staying motivated and on track is also easier when you can check back in, see your progress and realize the steps you’re taking are making an impact. Checking in every few months to see how you can grow gives you the chance to celebrate your progress, learn from challenges and keep building lasting habits that feel good.
To get started with personalized tips to set your own health goals, visit heart.org/mylifecheck.
Photos courtesy of Shutterstock
<img src="https://ssl.google-analytics.com/collect?v=1&tid=UA-482330-7&cid=1955551e-1975-5e52-0cdb-8516071094cd&sc=start&t=pageview&dl=http%3A%2F%2Ftrack.familyfeatures.com%2F17763%2F10236&dt=STACKING-HEALTHY-HABITS-FOR-PROGRESS-NOT-PERFECTION" />
<script src="https://erp.featureimpact.com/api/v1/tracking/17763/10236/track.js"></script>
<script type="text/javascript">
(function () {
var image = new Image(1, 1);
image.src = 'https://erp.featureimpact.com/api/v1/tracking/17763/10236/track.gif?referrer=' + window.location.href;
image.id = 'feature-impact-content-tracking-pixel';
image.style.position = 'absolute';
image.style.top = 0;
image.style.left = 0;
document.body.appendChild(image);
})();
</script>SOURCE:
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
