Health
Understanding a Treatment Option for Advanced Kidney Cancer

(Family Features) When kidney cancer spreads or becomes advanced, it can be challenging to treat. Common signs and symptoms can include blood in urine, lower back pain on one side, a mass on the side or lower back, loss of appetite or unexplained weight loss.
While a diagnosis of advanced kidney cancer can be overwhelming, there are steps patients can take to feel more empowered as they face the disease, starting with learning about the treatments that may be available for them.
Exploring Your Options
When facing advanced kidney cancer, it’s important for patients and caregivers to have open communication with their healthcare team to understand the diagnosis and establish a treatment plan.
Asking questions to understand where the cancer has spread, what the expected prognosis is and the potential benefits of treatment – including the possibility to live longer – can be critical to aligning on a path forward.
Fortunately, there are several types of medicines available for advanced kidney cancer today, depending on the specifics of each patient’s disease. Chemotherapy, targeted therapy or immunotherapy are a few types of treatment that may be considered, sometimes in combination. Immunotherapy works differently than chemotherapy or targeted therapy, as it helps a person’s own immune system to fight cancer and can enable the immune system to find and attack cancer cells. For some patients, dual immunotherapy – or a combination of two immunotherapy treatments – may be recommended.
For example, Opdivo (nivolumab) + Yervoy (ipilimumab) is approved by the U.S. Food and Drug Administration (FDA) as a combination of two immunotherapies for certain newly diagnosed adults whose kidney cancer (also referred to as renal cell carcinoma) has spread. It is not known if Opdivo is safe and effective in children younger than 18 years of age. Opdivo (10 mg/mL) and Yervoy (5 mg/mL) are injections for intravenous use.
This combination of two immunotherapies has the potential to work with the immune system in different but complementary ways to help fight cancer. While Yervoy may stimulate the kind of cells that help fight cancer, Opdivo may help these cells find and fight the cancer cells again.
While doing so, this immunotherapy combination can also affect healthy cells. These problems can sometimes become serious or life threatening and can lead to death. These problems may happen anytime during treatment or even after treatment has ended. You may have more than one of these problems at the same time. Some of these problems may happen more often when Opdivo is used in combination with Yervoy.
Opdivo and Yervoy can cause problems that can sometimes become serious or life-threatening and can lead to death. Serious side effects may include lung problems; intestinal problems; liver problems; hormone gland problems; kidney problems; skin problems; eye problems; problems in other organs and tissues; severe infusion reactions; and complications of stem cell transplant, including graft-versus-host disease (GVHD), that uses donor stem cells (allogeneic). Call or see your healthcare provider right away for any new or worsening signs or symptoms. Please see additional Important Safety Information below.
Understanding Overall Survival
One of the most important considerations for choosing a treatment is the potential for survival, or the chance to live longer. Overall survival is sometimes reported as a survival rate, which is the percentage of people in a clinical trial who are still alive for a certain time period after being diagnosed with or starting treatment for a disease, such as cancer.
“After my cancer diagnosis, my wife and I prayed about our future and pursuing every avenue with that goal in mind,” said Terry Broussard, who has been living with advanced kidney cancer. “I wanted a treatment that may give me a chance to live longer in order to see my youngest child graduate high school.”
Broussard’s doctor recommended treatment with Opdivo + Yervoy, which has overall survival data at five years. The FDA approval of this dual immunotherapy in advanced renal cell carcinoma (RCC) was based on results from the CheckMate -214 clinical trial, which included 847 previously untreated patients with kidney cancer that had spread and with one or more risk factors.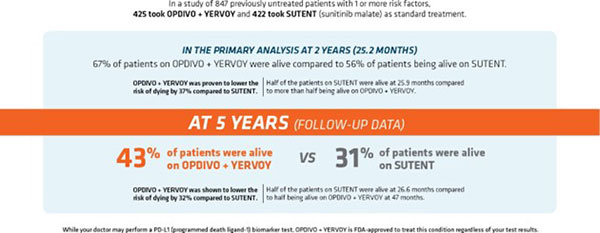
In the primary analysis at two years (25.2 months), the length of time patients lived without tumors worsening was 11.6 months for this immunotherapy combination and 8.4 months for sunitinib. There was no meaningful difference between the two treatments.
Researchers also assessed the overall response rate, which is a measure of the percentage of patients whose cancer shrunk (partial response) or disappeared completely (complete response) after treatment.
At the two-year time point, 41.6% of patients treated with Opdivo + Yervoy (95% CI:36.9-46.5) responded to treatment (n=177/425) versus 26.5% (n=112/422) of those treated with sunitinib (95% CI:22.4-31.0). Partial tumor shrinkage occurred in 32.2% of the patients treated with this immunotherapy combination compared to 25.4% of those treated with sunitinib. Tumors disappeared completely in 9.4% of patients treated with this immunotherapy combination versus in 1.2% of patients treated with sunitinib. The disappearance of any measurable tumors in response to treatment does not necessarily mean the cancer has been cured. Opdivo + Yervoy will not work for everyone. Individual results may vary.
“Advanced kidney cancer is a complex disease with many treatment options, which can feel overwhelming for people facing a devastating cancer diagnosis,” said Ulka Vaishampayan, M.D., professor, Internal Medicine, Division of Hematology/Oncology, University of Michigan. “The goal of treatment is to help patients live longer, and research like these five-year data gives us insight into what treatment with Opdivo + Yervoy may look like for patients from the trial over time.”
The most common side effects of Opdivo, when used in combination with Yervoy, include: feeling tired; diarrhea; rash; itching; nausea; pain in muscles, bones, and joints; fever; cough; decreased appetite; vomiting; stomach-area (abdominal) pain; shortness of breath; upper respiratory tract infection; headache; low thyroid hormone levels (hypothyroidism); constipation; decreased weight; and dizziness.
Establishing and Leaning on a Support System
From diagnosis to treatment and beyond, many patients find the support from family, friends and loved ones invaluable. Identifying a friend, spouse or caregiver who can join doctor appointments, ask questions and take notes can be a helpful way to track all the details that can often be overwhelming when facing cancer. “I’ve been incredibly lucky to have the support of my wife, children, nurses and doctors every step of the way,” said Broussard. “Even in the most challenging moments, knowing they were by my side gave me the hope and inspiration I needed to continue moving forward.”
To learn more, visit Opdivo.com.
Source: Bristol Myers Squibb
Photo caption: Terry Broussard and his wife, Tracy. Broussard is an actual patient who has been compensated by Bristol Myers Squibb for his time.
INDICATION AND IMPORTANT SAFETY INFORMATION
OPDIVO® (nivolumab) is a prescription medicine used in combination with YERVOY® (ipilimumab) to treat adults with kidney cancer in certain people when your cancer has spread (advanced renal cell carcinoma) and you have not already had treatment for your advanced RCC.
It is not known if OPDIVO is safe and effective in children younger than 18 years of age.
Information provided in this article is not a substitute for talking with your healthcare professional. Your healthcare professional is the best source of information about your disease.
Important Safety Information for OPDIVO® (nivolumab) + YERVOY® (ipilimumab)
What is the most important information I should know about OPDIVO + YERVOY?
OPDIVO and YERVOY are medicines that may treat certain cancers by working with your immune system. OPDIVO and YERVOY can cause your immune system to attack normal organs and tissues in any area of your body and can affect the way they work. These problems can sometimes become severe or life-threatening and can lead to death. These problems may happen anytime during treatment or even after your treatment has ended. You may have more than one of these problems at the same time. Some of these problems may happen more often when OPDIVO is used in combination with another therapy.
What are the serious side effects of OPDIVO + YERVOY?
Call or see your healthcare provider right away if you develop any new or worse signs or symptoms, including:
- Lung problems: new or worsening cough; shortness of breath; chest pain
- Intestinal problems: diarrhea (loose stools) or more frequent bowel movements than usual; stools that are black, tarry, sticky, or have blood or mucus; severe stomach-area (abdominal) pain or tenderness
- Liver problems: yellowing of your skin or the whites of your eyes; severe nausea or vomiting; pain on the right side of your stomach area (abdomen); dark urine (tea colored); bleeding or bruising more easily than normal
- Hormone gland problems: headaches that will not go away or unusual headaches; eye sensitivity to light; eye problems; rapid heart beat; increased sweating; extreme tiredness; weight gain or weight loss; feeling more hungry or thirsty than usual; urinating more often than usual; hair loss; feeling cold; constipation; your voice gets deeper; dizziness or fainting; changes in mood or behavior, such as decreased sex drive, irritability, or forgetfulness
- Kidney problems: decrease in your amount of urine; blood in your urine; swelling in your ankles; loss of appetite
- Skin problems: rash; itching; skin blistering or peeling; painful sores or ulcers in the mouth or nose, throat, or genital area
- Eye problems: blurry vision, double vision, or other vision problems; eye pain or redness.
Problems can also happen in other organs and tissues. These are not all of the signs and symptoms of immune system problems that can happen with OPDIVO and YERVOY. Call or see your healthcare provider right away for any new or worsening signs or symptoms, which may include:
- Chest pain; irregular heart beat; shortness of breath; swelling of ankles
- Confusion; sleepiness; memory problems; changes in mood or behavior; stiff neck; balance problems; tingling or numbness of the arms or legs
- Double vision; blurry vision; sensitivity to light; eye pain; changes in eye sight
- Persistent or severe muscle pain or weakness; muscle cramps
- Low red blood cells; bruising
Getting medical help right away may help keep these problems from becoming more serious. Your healthcare team will check you for these problems during treatment and may treat you with corticosteroid or hormone replacement medicines. Your healthcare team may also need to delay or completely stop your treatment if you have severe side effects.
Possible side effects of OPDIVO + YERVOY
OPDIVO and OPDIVO + YERVOY can cause serious side effects, including:
- See “What is the most important information I should know about OPDIVO + YERVOY?”
- Severe infusion reactions. Tell your healthcare team right away if you get these symptoms during an infusion of OPDIVO or YERVOY: chills or shaking; itching or rash; flushing; shortness of breath or wheezing; dizziness; feel like passing out; fever; back or neck pain
- Complications, including graft-versus-host disease (GVHD), of bone marrow (stem cell) transplant that uses donor stem cells (allogeneic). These complications can be severe and can lead to death. These complications may happen if you underwent transplantation either before or after being treated with OPDIVO or YERVOY. Your healthcare provider will monitor you for these complications.
The most common side effects of OPDIVO, when used in combination with YERVOY, include: feeling tired; diarrhea; rash; itching; nausea; pain in muscles, bones, and joints; fever; cough; decreased appetite; vomiting; stomach-area (abdominal) pain; shortness of breath; upper respiratory tract infection; headache; low thyroid hormone levels (hypothyroidism); constipation; decreased weight; and dizziness.
These are not all the possible side effects. For more information, ask your healthcare provider or pharmacist. You are encouraged to report side effects of prescription drugs to the FDA. Call 1-800-FDA- 1088.
Before receiving OPDIVO or YERVOY, tell your healthcare provider about all of your medical conditions, including if you:
- have immune system problems such as Crohn’s disease, ulcerative colitis, or lupus
- have received an organ transplant
- have received or plan to receive a stem cell transplant that uses donor stem cells (allogeneic)
- have received radiation treatment to your chest area in the past and have received other medicines that are like OPDIVO
- have a condition that affects your nervous system, such as myasthenia gravis or Guillain-Barré syndrome
- are pregnant or plan to become pregnant. OPDIVO and YERVOY can harm your unborn baby
- are breastfeeding or plan to breastfeed. It is not known if OPDIVO or YERVOY passes into your breast milk. Do not breastfeed during treatment with OPDIVO or YERVOY and for 5 months after the last dose of OPDIVO or YERVOY.
Females who are able to become pregnant:
Your healthcare provider should do a pregnancy test before you start receiving OPDIVO or YERVOY.
- You should use an effective method of birth control during your treatment and for at least 5 months after the last dose of OPDIVO or YERVOY. Talk to your healthcare provider about birth control methods that you can use during this time.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with OPDIVO or YERVOY. You or your healthcare provider should contact Bristol-Myers Squibb at 1-844-593-7869 as soon as you become aware of a pregnancy.
Tell your healthcare provider about all the medicines you take, including prescription and over-the- counter medicines, vitamins, and herbal supplements.
Please see U.S. Full Prescribing Information and Medication Guide for OPDIVO and YERVOY.
© 2023 Bristol-Myers Squibb Company. All Rights Reserved.
OPDIVO® and YERVOY® are registered trademarks of Bristol-Myers Squibb Company.
7356-US-2200719 2/23
SOURCE:
Bristol Myers Squibb
https://stmdailynews.com/category/lifestyle/health-and-wellness/
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
Lifestyle
How to Practice Thoughtful Grief Etiquette Online
Grief experts advise caution in sharing condolences and loss-related information on social media, emphasizing the importance of prioritizing the grieving family’s needs. Thoughtful posting practices include waiting for family approval, reaching out privately first, and avoiding speculation about the cause of death. Compassionate communication is essential in these sensitive situations.

(Feature Impact) News of a death can spread online in seconds – often before families have notified close family members privately. That’s why grief experts urge people to rethink how they share condolences, tributes and loss-related information on social media, particularly during the winter months when grief can feel especially isolating.
“Grief etiquette is about putting the needs of the grieving family first, not our urge to say something publicly,” said Dr. Camelia L. Clarke, National Funeral Directors Association (NFDA) spokesperson, funeral director and grief educator with nearly 30 years of experience. “Just because information can be shared instantly doesn’t mean it should be.”
Social media has become a common place for sharing condolences, tributes and memories. However, grief experts caution that, without thoughtful consideration, online posts can unintentionally cause harm. Knowing when to post, what to say and when to remain silent can make a meaningful difference for families experiencing loss.
Consider this advice from the experts at the NFDA.
Grief Etiquette in the Digital Age
Grief etiquette refers to the unspoken guidelines for how individuals acknowledge death, loss and mourning, particularly online.
According to Clarke, one of the most important principles is restraint.
“When a death is shared online too quickly, families can feel exposed and overwhelmed at a moment when they’re still processing the loss themselves,” she said. “Waiting is an act of compassion.”
Best Practices for Posting About Loss Online
As social media continues to play a role in modern mourning, grief professionals encourage users to pause before posting and consider a few key guidelines:
- Let the family lead. Don’t post about a death until the immediate family has made it public.
- Ask permission. Obtain consent before sharing photos, stories or tributes.
- Reach out privately first. A direct message, call or handwritten note can be more meaningful than a public comment.
- Avoid speculation. Don’t ask about or share details regarding the cause of death.
- Offer ongoing support. Grief extends far beyond the first days or weeks after a loss.
What to Say (and Avoid)
When expressing condolences online, experts recommend simplicity, sincerity and sensitivity. Messages that acknowledge loss without attempting to explain or minimize it are often the most supportive.
Helpful phrases include:
- “I’m sorry for your loss.”
- “Thinking of you and your family.”
- “I’m here if you want to talk or need anything.”
By contrast, well-meaning cliches can unintentionally cause harm. Phrases such as “They’re in a better place” or “Everything happens for a reason” may reflect the speaker’s beliefs, but they can feel dismissive to someone grieving.
“Grieving people don’t need answers – they need presence,” Clarke said. “Listening matters more than saying the perfect thing.”
Resources for Families and Friends
As digital spaces continue to shape how people communicate during life’s most difficult moments, experts agree empathy, patience and respect remain timeless.
“Grief is deeply personal,” Clarke said. “When we slow down and lead with compassion, we honor both the person who has died and those who are left to grieve.”
To learn more about how to support a grieving person and access free, expert-reviewed resources for navigating grief, expressing condolences and supporting loved ones before, during and after a loss, visit RememberingALife.com, an initiative of the NFDA.
Photo courtesy of Shutterstock
<img src="https://ssl.google-analytics.com/collect?v=1&tid=UA-482330-7&cid=1955551e-1975-5e52-0cdb-8516071094cd&sc=start&t=pageview&dl=http%3A%2F%2Ftrack.familyfeatures.com%2F17832%2F10240&dt=HOW-TO-PRACTICE-THOUGHTFUL-GRIEF-ETIQUETTE-ONLINE" />
<img src="https://erp.featureimpact.com/api/v1/tracking/17832/10240/track.gif" />SOURCE:
National Funeral Directors Association
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
Food and Beverage
Fresh Thinking About Frozen: Bring Quality Meals to the Table While Cutting Food Waste and Stretching Your Budget
For many families, the freezer is for last-minute meal options. However, new federal nutrition guidance and growing scientific consensus reveal a different reality: frozen foods can be the starting point for healthy eating, not a backup plan.
Last Updated on February 21, 2026 by Daily News Staff
(Feature Impact) The key to easy preparation of high-quality meals, wasting less food and saving money may already be sitting in your kitchen.
For many families, the freezer is for last-minute meal options. However, new federal nutrition guidance and growing scientific consensus reveal a different reality: frozen foods can be the starting point for healthy eating, not a backup plan. That’s why the American Frozen Food Institute (AFFI) is launching “Fresh Thinking About Frozen,” a campaign to help families discover these benefits of frozen foods.
Making Nutrition Achievable
The recently released 2025-2030 Dietary Guidelines for Americans, the nation’s top nutrition advice, emphasizes portion control and nutrient-dense foods. Frozen options deliver on both counts.
Families who keep frozen produce on hand tend to eat more fruits and vegetables overall. Pre-portioned frozen meals also help people eat what they need without overdoing it. Plus, the convenience factor matters: frozen berries are ready for a morning smoothie, pre-cut frozen vegetables can be added to tonight’s stir-fry and a balanced frozen meal can be quickly paired with a salad.
That isn’t cutting corners. It’s being smart on how best to feed a family well.
Freezing Hits the Pause Button on Fresh Foods
Freezing food only changes a food’s temperature, not its nutrition. Freezing keeps food close to its original state without requiring additives.
Produce begins to lose nutritional value right after it’s harvested. Freezing fruits and vegetables hours after harvest pauses nutrient degradation and locks in the vitamins and minerals, so the food remains farm fresh even as it travels across the country to your grocery store. Frozen meals are similarly made with real ingredients and turned into just-cooked recipes then frozen for families to eat when they’re ready.
The nutrition community understands this. A recent survey conducted by AFFI found 94% of registered dietitians agree frozen fruits and vegetables are just as nutritious as their fresh counterparts. Another 92% said frozen foods offer a variety of nutritious meal offerings. These findings are central to the “Fresh Thinking About Frozen” message: Frozen is not second-best. It’s simply smart.
Solving the Food Waste Problem
Nearly 40% of food in the United States gets thrown away, according to the nonprofit ReFED. That translates to roughly $1,500 per year per household, straight into the trash along with unused produce and forgotten leftovers.
Frozen helps fix that problem. Eight in 10 consumers agree buying frozen helps reduce food waste at home, AFFI research finds. The reason is simple: You use what you need, when you need it and the rest stays perfectly preserved. No more dreading the refrigerator cleanouts and feeling guilty over the uneaten food going into the trashcan.
Time for Fresh Thinking
Families already making this shift aren’t settling for less. They’re strategic about nutrition, budget and time. They integrate the freezer into regular meal planning. They feel confident about providing quality foods that are simply frozen.
The freezer isn’t a place of last resort. It’s a tool for eating well in real life. Visit frozenadvantage.org/FTAF for tips, recipes and resources to make the most of your freezer.
Photos courtesy of Shutterstock
SOURCE:
American Frozen Food Institute
At our core, we at STM Daily News, strive to keep you informed and inspired with the freshest content on all things food and beverage. From mouthwatering recipes to intriguing articles, we’re here to satisfy your appetite for culinary knowledge.
Visit our Food & Drink section to get the latest on Foodie News and recipes, offering a delightful blend of culinary inspiration and gastronomic trends to elevate your dining experience. https://stmdailynews.com/food-and-drink/
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
health and wellness
Stacking Healthy Habits for Progress, Not Perfection
Healthy Habits: Many struggle with building healthier habits due to unrealistic expectations rather than lack of motivation. The American Heart Association’s My Life Check tool offers personalized heart health insights, helping to set attainable goals. Simple lifestyle changes—focused on nutrition, movement, sleep, and stress management—can gradually lead to significant health improvements.

(Feature Impact) Despite the best of intentions, it’s common for plans to build healthier habits to fall flat. Often, the culprit isn’t a lack of motivation or discipline; rather, it’s unrealistic expectations.
Overhauling your lifestyle requires a level of commitment that isn’t always practical. Understanding your personal health needs and the challenges you need to overcome can help give you a more realistic roadmap toward better health.
Tools to Guide You
Every plan needs a starting point and there are many reputable sources that can help guide you toward a plan that addresses your personal health needs.
For example, the American Heart Association introduced My Life Check, a simple, free tool to help individuals understand their heart health and what’s driving it. Users answer simple questions about their daily habits and health factors to get a personalized Heart Health Score in minutes.
The results are private and downloadable, giving you full control of your information. The tool turns big goals into small, specific actions you can start right away. Knowing your numbers relative to your heart health (and where you are in comparison to target ranges for optimal health) can help you decide how to build a better map to get you where you want to be.
While the report is customized to each individual, no personal data is stored and answers are only used to calculate health scores and provide personalized recommendations and practical steps to improve your health, so you can use your results to focus on what matters most to you. Every small step you take, such as moving more, eating smarter, sleeping better or managing stress, can add up over time.
Finding Your Path
Once you’re armed with data and know where you stand on your heart health numbers, small steps become clearer and more manageable. That knowledge makes it easier to choose one area to focus on, such as getting more sleep, taking daily walks or adding more color to your meals.
Healthy changes don’t need to be expensive or complicated. The best habits are ones that fit real life when every action you take moves you closer to your goals.
Eat Smart
Choose foods that help you feel your best, one meal at a time. Add more color to your plate and focus on balance, not restriction. Simple, affordable swaps can make a real difference.
Move More
Find movement that fits your life, such as a walk, a stretch or dancing while you cook. Every bit of activity counts and it all supports your heart and mind. Move for joy, not just for results.
Sleep Well
Rest is a foundation of good health, not a reward. Protect your bedtime routine and give your body the recovery it deserves. Notice how good sleep makes everything else easier.
Manage Stress
Check in with yourself regularly, both mentally and emotionally. Create simple moments to pause, breathe, laugh or step outside. Connection, kindness and calm all support a healthy heart.
Staying motivated and on track is also easier when you can check back in, see your progress and realize the steps you’re taking are making an impact. Checking in every few months to see how you can grow gives you the chance to celebrate your progress, learn from challenges and keep building lasting habits that feel good.
To get started with personalized tips to set your own health goals, visit heart.org/mylifecheck.
Photos courtesy of Shutterstock
<img src="https://ssl.google-analytics.com/collect?v=1&tid=UA-482330-7&cid=1955551e-1975-5e52-0cdb-8516071094cd&sc=start&t=pageview&dl=http%3A%2F%2Ftrack.familyfeatures.com%2F17763%2F10236&dt=STACKING-HEALTHY-HABITS-FOR-PROGRESS-NOT-PERFECTION" />
<script src="https://erp.featureimpact.com/api/v1/tracking/17763/10236/track.js"></script>
<script type="text/javascript">
(function () {
var image = new Image(1, 1);
image.src = 'https://erp.featureimpact.com/api/v1/tracking/17763/10236/track.gif?referrer=' + window.location.href;
image.id = 'feature-impact-content-tracking-pixel';
image.style.position = 'absolute';
image.style.top = 0;
image.style.left = 0;
document.body.appendChild(image);
})();
</script>SOURCE:
Discover more from Daily News
Subscribe to get the latest posts sent to your email.
